When Quiet is Too Quiet
Hello my name is Nikki I’m a proud Mum to 4 handsome boys. I moved to Grimsby just over 10 years ago after spending a number of years studying and working in various cities but was originally born and raised in Newcastle.  I am an optimistic person who looks for the positives and hopes always that change is for the better. I believe in fairness, equality, inclusion, teamwork and of course kindness. My family are most important to. We particularly enjoy holidays where we can relax and enjoy the time together without distraction. Life should be fun and we try to keep that balance. In my spare time I enjoy nature and reading. With over 20 years of nursing experience and as a post-graduate in biology and psychology it was shocking to discover I had a child with a hidden disability living right under my nose.
I am an optimistic person who looks for the positives and hopes always that change is for the better. I believe in fairness, equality, inclusion, teamwork and of course kindness. My family are most important to. We particularly enjoy holidays where we can relax and enjoy the time together without distraction. Life should be fun and we try to keep that balance. In my spare time I enjoy nature and reading. With over 20 years of nursing experience and as a post-graduate in biology and psychology it was shocking to discover I had a child with a hidden disability living right under my nose.
Although this was a number of years ago it still highlights the lack of awareness and training in SM provided to professionals. My passion has come from our experience and with an increase in anxiety disorders in general I strive to bring about awareness of SM with an ultimate aim:-
- For C/YP to be identified early so they can benefit from early intervention.
- Raise public awareness so those with SM feel accepted and need not suffer the affect of misunderstandings.
- To share our story as I feel there is a valuable lesson to be learned.
- To offer support to anyone affected by SM so that they have what I needed at the beginning of our journey.
It’s important to me that people know there is hope and you can overcome SM.
When Quiet is Too Quiet
I was in my late 30’s before I even heard of the term selective mutism (SM), I was totally unaware it even existed. To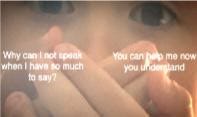 be honest if someone would have mentioned it to me earlier in life the concept would likely have left me with a puzzled expression, I certainly would not have felt the need to give it any further thought. However as I began to read I realised this was the moment everything changed…‘selective mutism is an anxiety disorder which affects communication in certain situations…’
be honest if someone would have mentioned it to me earlier in life the concept would likely have left me with a puzzled expression, I certainly would not have felt the need to give it any further thought. However as I began to read I realised this was the moment everything changed…‘selective mutism is an anxiety disorder which affects communication in certain situations…’
…Suddenly everything started to make sense, all the unusual behaviours, the unanswered questions, my confused thoughts rapidly cascaded together in one enlightening moment. I could finally see what our child had been going through and for the first time I really began to understand him.
Selective mutism was very real, this was my child and I had already seen the impact!
I sat for a while thinking memories suddenly flooding my mind of situations where SM stole the voice of my child. It explained why he wouldn’t say sorry for accidentally hurting his younger brother while playing or why he didn’t ask for ice-cream himself at the counter when it was something he so desperately wanted. He couldn’t, he was literally unable. It gave reason to why he would hide behind us in the park when we were approached by our friends, never responding to their greeting with eyes firmly to the ground, he wasn’t being rude in not answering, he simply couldn’t. When asked a question I recall him whispering behind his hand so others couldn’t hear and all the times he’d stare pleadingly into my eyes, biting his lip whilst awaiting my rescue. Not because he was shy, no this is SM. Ispoke to my husband and he confirmed my thoughts. How had we not realised? Combined with this relief and new knowledge came floods of guilt and many more questions.
This was the beginning of our journey, an unforeseen experience that has taught us far more than we could ever have anticipated. Abruptly we felt thrown into this new world. The beginning of special educational needs, educational health care plans and mental health meetings. I can’t lie, it’s been the most exhausting, emotional rollercoaster I could ever have imagined.
Our son was now a teenager who on reflection had been misunderstood for so many years. He must have suffered unnecessarily and now desperately needed our help. We blamed each other, we blamed others and we felt sad that our son was unable to talk to us about his difficulties. My heart hurt so much for him and I felt an overwhelming need to put things right, to get back the happy jovial boy we once knew.
I searched desperately in an attempt to find someone locally with the experience and knowledge that could help. Determined I thought about nothing else,holding on in hope as I exhausted every avenue. It was to no avail and feeling alone and despondent, once again I had failed my son. Thankfully I had joined an on-line support group and after finding a specialist out of the area I finally had someone offering hope. It was at that point I realised just how common SM was and sadly it also became apparent just how familiar our story sounded.
So what exactly is SM?
SM is described in the DSM-V (a diagnostic manual of mental disorders) as a severe anxiety disorder. The criteria for diagnosis includes a persistent lack of speech where expected with a duration of over one month. It must be affecting educational, occupational or social communication and cannot be due to a lack of comfort with the language used. It is estimated that over 1:140 children have SM and can be seen in individuals as young as 2-3 years but is mostly noticed around age 5 when they enter school. Early recognition and interventions is key to helping young children as left untreated it can become far more difficult to overcome as behaviours become further entrenched and can persist into adulthood. There are vast regional variations in support available sometimes this comes from educational psychologists, speech and language therapists or mental health care practitioners. However it is clear that what is more important and required is the experience of SM which is essential when seeking help, not which professional takes the lead.
SM is extremely complex and each individual’s ability to communicate will vary within different contexts. This may mean that a person may be able to speak with someone well in one situation but not in another. Others may not speak if they are conscious of being overheard or they might find speaking to peers harder than adults, strangers easier than colleagues. Regardless of when SM occurs, if individuals feel pressured to talk, are uncomfortable or have expectations placed upon them, they may become literally ‘stuck for words’ and be unable to speak, caused by overwhelming anxiety. Difficulty to communicate is not only limited to speech it can include non-verbal forms of communication, initiation and sometimes involvement in activities which draw attention. SM and Social anxiety disorder are often diagnosed together. Maggie Johnson and Alison Wintgens describe SM in the selective mutism manual as two profiles:
- High profile is the most obvious and easiest to recognise and diagnose, individuals are unable to speak when speech is normally expected.
- Low profile SM is more likely to be perceived as shy, they present as reluctant to talk and they may answer with a single word, a changed voice or short answer but this is not without anxiety, (It is thought the consequences for not speaking outweighs the anxiety of speaking).
With both profiles the lack of understanding as to why individuals who are physically able to speak do not can lead to frustration, and confusion. These include a belief that the person is manipulative, rude, deliberately avoiding engaging or are oppositional. Some believe it is caused by trauma but traumatic mutism is a completely different diagnosis. It’s interesting to know that SM is not new, it was first observed in 1877 by a German physician called Adolph Kussmaul who named it aphasia voluntaria it was later changed to elective mutism in 1934 by a child psychologist Moritz Tramer who was working in Switzerland with psychiatric and emotionally disturbed children. During this period it was believed that mutism was a refusal to speak. It wasn’t until knowledge improved recognising SM manifested from anxiety that the term was changed to selective mutism back in the mid 1990’s to represent how speech is affected in select situations. Unfortunately the term selective can also be interpreted as a choice in selecting who or when to speak, with that in mind many people today prefer using the term situational mutism.
The familiar situation that I encountered was that of a child who was seen as shy or difficult who didn’t get recognised as having difficulties until it was too late. They had reached their teens and the added social pressures during adolescence, feeling different and maintaining academic performance rendered them isolated and withdrawn they had reached breaking point. You wonder how on earth this could happen but like the quote by Socrates states ‘We don’t know what we don’t know’. It is only with hindsight do we see the red flags and of course if we could go back would handle things differently.
For us home life initially seemed fine, our children would take part in various activities, they would have friends for tea, play out, and visit extended family. We assumed our son’s reluctance to speak with strangers or friends was simply shyness. After all as a child I too was considered shy and disliked too much attention, it was accepted as part of him and the way he’d always been. As a youngster at the age of 2-3 years he didn’t speak in nursery, he only went a few days a week and thought this was the reason. By the time he was in school he had made some good friends and was liked by many for his jovial ways, yet on reflection he was unable to ask staff for help. We moved areas at the end of year 2, he was excited but reluctant to go to his new school. It took a long time for him to settle and each morning separation was difficult, yet I was reassured he was fine. He made some new friends and seemed happy at pick up.
Many educators I’m sure are more than familiar with the quiet student that never puts up a hand to volunteer information, doesn’t shout the answers out in class or tell anything personal about life outside of school. They are the quiet, no fuss compliant pupils who get on with the work and cause little need for concern.
This was my child at school. He would answer the register, nod and shake his head or simply just shrug his shoulders. He was the child that would just keep his head down and look like he was getting on with the task set. For most learners that’s not a problem it’s just their personality, but in our son’s case his quiet was too quiet. Not asking for help, speaking less and less he learnt the art of avoidance and slipped way under the radar which is exactly where he wanted to be, no pressure and no attention. He had acquired the ability to mask.
After transferring to secondary school with increasing demands his anxiety escalated adding pressure to his mental health. To his peers he had adopted the persona of the ‘boy who doesn’t speak’, he was ignored by many and those that did speak soon gave up. He missed many opportunities to practice social skills and develop independence and refused to join activities. Although he doesn’t talk about this he has had many negative comments passed sometimes innocently but not without consequence and was left very vulnerable to bullying. Eventually he became explosive to any requests once home from school, he had difficulty sleeping, was hyper vigilant and on survival mode 24/7. He withdrew to his room, isolated, and became unable to speak to extended family and people he had once been able to. It was at this point we thankfully learnt of SM and addressed the situation he was eventually diagnosed autistic along with other anxiety disorders.
Helping children overcome SM varies with age and abilities but primarily starts with providing the right setting. The focus initially should be on lowering the anxiety surrounding speech by providing a nurturing environment and giving the opportunity to engage with no pressure to speak. This can be achieved by allowing alternative ways to communicate, giving extra time to respond, building rapport, using humour, gestures and interests as a motivator. For educators, providing the smallest accommodations in class can make the biggest difference! Avoid surprises, placing them on the spot or anything that draws attention making them stand out. For more severe and complex SM seeking help from trained professionals may also be required, cognitive behavioural therapy, graded exposure and stimulus fading can help and in some cases medication may be used.
Like ourselves at the beginning most people we encountered did not understand SM and I found myself constantly explaining and educating. If I’m honest this is something I am quite passionate about and don’t mind doing. I often get that perplexed expression or look of disbelief as frustratingly they are not able to observe the SM from both sides and subsequently only get to see half a picture. From my perspective it is really like living with two completely different people.
I can’t change the past and the impact it had on my son but we can learn from it! I hope by sharing our experience this may one day help another, so if you have any concerns please discuss them with colleagues and parents.
I want you to know that it’s never too late to begin the journey to recovery, no matter how bad anxiety may seem today, it can get better.
My son is moving forward one manageable step at a time and that’s what is needed right now, no pressure, no expectations, just time. Today he is happier enjoying life. He has reminded us about the important things that are too often missed in this busy world. We take pleasure in achievements no matter how small. I am like any mother so proud of what he has achieved despite all the barriers he’s faced he is much stronger than he knows. Yes, he will still have many challenges ahead but his SM is not just one for him to overcome, but one for society to better understand and when the environment is right you will see him and all his abilities. His voice need not be with words, for if it is not with words he is always comfortable. We are all different, we should be accepting of all our differences.
I would like to thank Andrew very much for this fantastic opportunity to write about SM and our journey of which I feel extremely honoured. I truly am grateful to have met so many wonderful people passionate in their work and friends for all their support over the years. Apologies for the length of this and if you’ve managed to get this far thank you so much for reading. Stay safe everyone.
By a Mum on a mission to raise the profile of Selective Mutism because it really does matter.
If you would like further information please visit:-
http://www.selectivemutism.org.uk- Selective Mutism Information and Research Association website
http://www.nhs.uk(A-Z Health)
http://www.thecommunicationtrust.org.uk http://www.icancharity.org.uk http://afasic.org.uk http://www.ispeak.org.uk http://www.selectivemutismcentre.org
Reading:- Johnson, M and Wintgens, A (2016) The Selective Mutism Resource Manual 2ndEdition. London. Speechmark.
