This really is exciting and great value…
New monthly subscription service Only £20 (ex vat)
Each month you will receive a 45 – 75 minute workshop video on a range of Special Educational subjects, including:
-
ADHD
-
Autism
-
Dyslexia
-
PDA (Pathological Demand Avoidance)
-
Attachment Disorder
-
Dyscalculia
-
Dyspraxia
-
Foetal Alcohol Spectrum Disorder
-
Gifted Talented Able
-
Positive Behaviour Support
All of these workshops come with directed tasks (homework) which I will feedback personally.
Normally priced at £50 per workshop, you only pay £20 (ex vat) per month to receive your monthly video (and lots of other goodies).
These video workshops are perfect for Continuing Professional Development (CPD) and Personal Development.
You will also receive access to articles and book extracts.
You will receive early access to forthcoming live and online events.
Something extra every week.
-
Patron-only updates
-
Early access
Check it out Here:
 Welcome to my book. My name is Andrew, and I am a consultant and trainer in the field of Neurological Diversity. I am a TEDx Speaker, Bamford Lecturer, prolific conference speaker and I am contracted to multiple organisations including universities, local authorities, and training consortiums. I deliver live workshops, digital workshops, in-service training, and focused classroom observations… and I have Attention Deficit Hyperactivity Disorder (ADHD). People have often asked me over the years why I do not have a book out. Well, the simple answer is that up until now I have not had anything to write about. But now I have. You see, I didn’t want to write yet another book about ADHD. If I was going to write about ADHD, I wanted it to have a purpose.
Welcome to my book. My name is Andrew, and I am a consultant and trainer in the field of Neurological Diversity. I am a TEDx Speaker, Bamford Lecturer, prolific conference speaker and I am contracted to multiple organisations including universities, local authorities, and training consortiums. I deliver live workshops, digital workshops, in-service training, and focused classroom observations… and I have Attention Deficit Hyperactivity Disorder (ADHD). People have often asked me over the years why I do not have a book out. Well, the simple answer is that up until now I have not had anything to write about. But now I have. You see, I didn’t want to write yet another book about ADHD. If I was going to write about ADHD, I wanted it to have a purpose.
So here it is, my purpose…
I am going to share with you my ADHD experience. It’s a complicated old story because I never really found out about my ADHD until my early 50s and it wasn’t until I was 53 that I received my diagnosis of Severe ADHD and therefore, I have spent the majority of my life so far wondering why I didn’t quite sit flush with the people around me. I knew that my brain was different to other people’s brains because… it just felt like that. I spent a great deal of my time not fitting in and wondering why I could never fit in, and actually being deeply upset about this peculiar state of being. Now I want to make a couple of things clear. Like I said, this is about my ADHD experience, not yours, your son’s or your daughter’s, or anybody else’s. We are all unique in our neurodiversity, and one thing I’ve learned in the day job is that there is no step by step manual on how to educate, live with or love a person with ADHD. In fact, I would go so far as to say that the minute you think you have developed a system for ADHD (or Autism, Dyslexia, Pathological Demand Avoidance and any other neurodiversity for that matter), you will have failed, simply because you are not dealing with a type, you are dealing with individuals. Having said all that, I will talk about the ADHD community as being ‘we’ or ‘us’. This is because although we are all different, there are certain attributes that most of us share. Furthermore, people with ADHD understand other people with ADHD (most of the time). I call it ‘The Brotherhood/Sisterhood’. I am always asking people if they are part of ‘The Brotherhood/Sisterhood’.
Every human being has a system for processing information and situations. This system is called ‘executive functioning’. People with ADHD have very different executive functioning processes to neurotypical people. Sometimes, I describe my executive functioning as ‘tiny bubbles’. Let me explain. When I am delivering a lecture, having a conversation, or, like now, writing a book, there is very little structure. It’s more like a stream of consciousness.
https://youtu.be/vJwRs0LdKTc
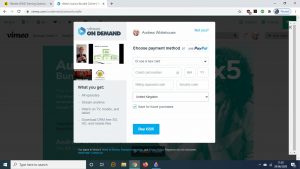
Go to www.andrewwhitehouse.co.uk
Scroll down and select subject
Choose either one module
Or a bundle
Click preview
Click buy
You will then receive your workshop(s)
If you receive the below, this means it is not uploaded as a bundle yet. But we do have it! Get in touch and we will get it to you ASAP.

Hello my name is Nikki I’m a proud Mum to 4 handsome boys. I moved to Grimsby just over 10 years ago after spending a number of years studying and working in various cities but was originally born and raised in Newcastle.  I am an optimistic person who looks for the positives and hopes always that change is for the better. I believe in fairness, equality, inclusion, teamwork and of course kindness. My family are most important to. We particularly enjoy holidays where we can relax and enjoy the time together without distraction. Life should be fun and we try to keep that balance. In my spare time I enjoy nature and reading. With over 20 years of nursing experience and as a post-graduate in biology and psychology it was shocking to discover I had a child with a hidden disability living right under my nose.
I am an optimistic person who looks for the positives and hopes always that change is for the better. I believe in fairness, equality, inclusion, teamwork and of course kindness. My family are most important to. We particularly enjoy holidays where we can relax and enjoy the time together without distraction. Life should be fun and we try to keep that balance. In my spare time I enjoy nature and reading. With over 20 years of nursing experience and as a post-graduate in biology and psychology it was shocking to discover I had a child with a hidden disability living right under my nose.
Although this was a number of years ago it still highlights the lack of awareness and training in SM provided to professionals. My passion has come from our experience and with an increase in anxiety disorders in general I strive to bring about awareness of SM with an ultimate aim:-
- For C/YP to be identified early so they can benefit from early intervention.
- Raise public awareness so those with SM feel accepted and need not suffer the affect of misunderstandings.
- To share our story as I feel there is a valuable lesson to be learned.
- To offer support to anyone affected by SM so that they have what I needed at the beginning of our journey.
It’s important to me that people know there is hope and you can overcome SM.
When Quiet is Too Quiet
I was in my late 30’s before I even heard of the term selective mutism (SM), I was totally unaware it even existed. To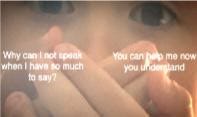 be honest if someone would have mentioned it to me earlier in life the concept would likely have left me with a puzzled expression, I certainly would not have felt the need to give it any further thought. However as I began to read I realised this was the moment everything changed…‘selective mutism is an anxiety disorder which affects communication in certain situations…’
be honest if someone would have mentioned it to me earlier in life the concept would likely have left me with a puzzled expression, I certainly would not have felt the need to give it any further thought. However as I began to read I realised this was the moment everything changed…‘selective mutism is an anxiety disorder which affects communication in certain situations…’
…Suddenly everything started to make sense, all the unusual behaviours, the unanswered questions, my confused thoughts rapidly cascaded together in one enlightening moment. I could finally see what our child had been going through and for the first time I really began to understand him.
Selective mutism was very real, this was my child and I had already seen the impact!
I sat for a while thinking memories suddenly flooding my mind of situations where SM stole the voice of my child. It explained why he wouldn’t say sorry for accidentally hurting his younger brother while playing or why he didn’t ask for ice-cream himself at the counter when it was something he so desperately wanted. He couldn’t, he was literally unable. It gave reason to why he would hide behind us in the park when we were approached by our friends, never responding to their greeting with eyes firmly to the ground, he wasn’t being rude in not answering, he simply couldn’t. When asked a question I recall him whispering behind his hand so others couldn’t hear and all the times he’d stare pleadingly into my eyes, biting his lip whilst awaiting my rescue. Not because he was shy, no this is SM. Ispoke to my husband and he confirmed my thoughts. How had we not realised? Combined with this relief and new knowledge came floods of guilt and many more questions.
This was the beginning of our journey, an unforeseen experience that has taught us far more than we could ever have anticipated. Abruptly we felt thrown into this new world. The beginning of special educational needs, educational health care plans and mental health meetings. I can’t lie, it’s been the most exhausting, emotional rollercoaster I could ever have imagined.
Our son was now a teenager who on reflection had been misunderstood for so many years. He must have suffered unnecessarily and now desperately needed our help. We blamed each other, we blamed others and we felt sad that our son was unable to talk to us about his difficulties. My heart hurt so much for him and I felt an overwhelming need to put things right, to get back the happy jovial boy we once knew.
I searched desperately in an attempt to find someone locally with the experience and knowledge that could help. Determined I thought about nothing else,holding on in hope as I exhausted every avenue. It was to no avail and feeling alone and despondent, once again I had failed my son. Thankfully I had joined an on-line support group and after finding a specialist out of the area I finally had someone offering hope. It was at that point I realised just how common SM was and sadly it also became apparent just how familiar our story sounded.
So what exactly is SM?
SM is described in the DSM-V (a diagnostic manual of mental disorders) as a severe anxiety disorder. The criteria for diagnosis includes a persistent lack of speech where expected with a duration of over one month. It must be affecting educational, occupational or social communication and cannot be due to a lack of comfort with the language used. It is estimated that over 1:140 children have SM and can be seen in individuals as young as 2-3 years but is mostly noticed around age 5 when they enter school. Early recognition and interventions is key to helping young children as left untreated it can become far more difficult to overcome as behaviours become further entrenched and can persist into adulthood. There are vast regional variations in support available sometimes this comes from educational psychologists, speech and language therapists or mental health care practitioners. However it is clear that what is more important and required is the experience of SM which is essential when seeking help, not which professional takes the lead.
SM is extremely complex and each individual’s ability to communicate will vary within different contexts. This may mean that a person may be able to speak with someone well in one situation but not in another. Others may not speak if they are conscious of being overheard or they might find speaking to peers harder than adults, strangers easier than colleagues. Regardless of when SM occurs, if individuals feel pressured to talk, are uncomfortable or have expectations placed upon them, they may become literally ‘stuck for words’ and be unable to speak, caused by overwhelming anxiety. Difficulty to communicate is not only limited to speech it can include non-verbal forms of communication, initiation and sometimes involvement in activities which draw attention. SM and Social anxiety disorder are often diagnosed together. Maggie Johnson and Alison Wintgens describe SM in the selective mutism manual as two profiles:
- High profile is the most obvious and easiest to recognise and diagnose, individuals are unable to speak when speech is normally expected.
- Low profile SM is more likely to be perceived as shy, they present as reluctant to talk and they may answer with a single word, a changed voice or short answer but this is not without anxiety, (It is thought the consequences for not speaking outweighs the anxiety of speaking).
With both profiles the lack of understanding as to why individuals who are physically able to speak do not can lead to frustration, and confusion. These include a belief that the person is manipulative, rude, deliberately avoiding engaging or are oppositional. Some believe it is caused by trauma but traumatic mutism is a completely different diagnosis. It’s interesting to know that SM is not new, it was first observed in 1877 by a German physician called Adolph Kussmaul who named it aphasia voluntaria it was later changed to elective mutism in 1934 by a child psychologist Moritz Tramer who was working in Switzerland with psychiatric and emotionally disturbed children. During this period it was believed that mutism was a refusal to speak. It wasn’t until knowledge improved recognising SM manifested from anxiety that the term was changed to selective mutism back in the mid 1990’s to represent how speech is affected in select situations. Unfortunately the term selective can also be interpreted as a choice in selecting who or when to speak, with that in mind many people today prefer using the term situational mutism.
The familiar situation that I encountered was that of a child who was seen as shy or difficult who didn’t get recognised as having difficulties until it was too late. They had reached their teens and the added social pressures during adolescence, feeling different and maintaining academic performance rendered them isolated and withdrawn they had reached breaking point. You wonder how on earth this could happen but like the quote by Socrates states ‘We don’t know what we don’t know’. It is only with hindsight do we see the red flags and of course if we could go back would handle things differently.
For us home life initially seemed fine, our children would take part in various activities, they would have friends for tea, play out, and visit extended family. We assumed our son’s reluctance to speak with strangers or friends was simply shyness. After all as a child I too was considered shy and disliked too much attention, it was accepted as part of him and the way he’d always been. As a youngster at the age of 2-3 years he didn’t speak in nursery, he only went a few days a week and thought this was the reason. By the time he was in school he had made some good friends and was liked by many for his jovial ways, yet on reflection he was unable to ask staff for help. We moved areas at the end of year 2, he was excited but reluctant to go to his new school. It took a long time for him to settle and each morning separation was difficult, yet I was reassured he was fine. He made some new friends and seemed happy at pick up.
Many educators I’m sure are more than familiar with the quiet student that never puts up a hand to volunteer information, doesn’t shout the answers out in class or tell anything personal about life outside of school. They are the quiet, no fuss compliant pupils who get on with the work and cause little need for concern.
This was my child at school. He would answer the register, nod and shake his head or simply just shrug his shoulders. He was the child that would just keep his head down and look like he was getting on with the task set. For most learners that’s not a problem it’s just their personality, but in our son’s case his quiet was too quiet. Not asking for help, speaking less and less he learnt the art of avoidance and slipped way under the radar which is exactly where he wanted to be, no pressure and no attention. He had acquired the ability to mask.
After transferring to secondary school with increasing demands his anxiety escalated adding pressure to his mental health. To his peers he had adopted the persona of the ‘boy who doesn’t speak’, he was ignored by many and those that did speak soon gave up. He missed many opportunities to practice social skills and develop independence and refused to join activities. Although he doesn’t talk about this he has had many negative comments passed sometimes innocently but not without consequence and was left very vulnerable to bullying. Eventually he became explosive to any requests once home from school, he had difficulty sleeping, was hyper vigilant and on survival mode 24/7. He withdrew to his room, isolated, and became unable to speak to extended family and people he had once been able to. It was at this point we thankfully learnt of SM and addressed the situation he was eventually diagnosed autistic along with other anxiety disorders.
Helping children overcome SM varies with age and abilities but primarily starts with providing the right setting. The focus initially should be on lowering the anxiety surrounding speech by providing a nurturing environment and giving the opportunity to engage with no pressure to speak. This can be achieved by allowing alternative ways to communicate, giving extra time to respond, building rapport, using humour, gestures and interests as a motivator. For educators, providing the smallest accommodations in class can make the biggest difference! Avoid surprises, placing them on the spot or anything that draws attention making them stand out. For more severe and complex SM seeking help from trained professionals may also be required, cognitive behavioural therapy, graded exposure and stimulus fading can help and in some cases medication may be used.
Like ourselves at the beginning most people we encountered did not understand SM and I found myself constantly explaining and educating. If I’m honest this is something I am quite passionate about and don’t mind doing. I often get that perplexed expression or look of disbelief as frustratingly they are not able to observe the SM from both sides and subsequently only get to see half a picture. From my perspective it is really like living with two completely different people.
I can’t change the past and the impact it had on my son but we can learn from it! I hope by sharing our experience this may one day help another, so if you have any concerns please discuss them with colleagues and parents.
I want you to know that it’s never too late to begin the journey to recovery, no matter how bad anxiety may seem today, it can get better.
My son is moving forward one manageable step at a time and that’s what is needed right now, no pressure, no expectations, just time. Today he is happier enjoying life. He has reminded us about the important things that are too often missed in this busy world. We take pleasure in achievements no matter how small. I am like any mother so proud of what he has achieved despite all the barriers he’s faced he is much stronger than he knows. Yes, he will still have many challenges ahead but his SM is not just one for him to overcome, but one for society to better understand and when the environment is right you will see him and all his abilities. His voice need not be with words, for if it is not with words he is always comfortable. We are all different, we should be accepting of all our differences.
I would like to thank Andrew very much for this fantastic opportunity to write about SM and our journey of which I feel extremely honoured. I truly am grateful to have met so many wonderful people passionate in their work and friends for all their support over the years. Apologies for the length of this and if you’ve managed to get this far thank you so much for reading. Stay safe everyone.
By a Mum on a mission to raise the profile of Selective Mutism because it really does matter.
If you would like further information please visit:-
http://www.selectivemutism.org.uk- Selective Mutism Information and Research Association website
http://www.nhs.uk(A-Z Health)
http://www.thecommunicationtrust.org.uk http://www.icancharity.org.uk http://afasic.org.uk http://www.ispeak.org.uk http://www.selectivemutismcentre.org
Reading:- Johnson, M and Wintgens, A (2016) The Selective Mutism Resource Manual 2ndEdition. London. Speechmark.
Voice From the Lockdown
As covid-19 sweeps the world, many governments have put their countries into lockdown
“So what are you doing while stuck at home Isaac?” You may ask…
well, I have done many new things since the lockdown.
Firstly, I have been filming and editing digitised courses for my dad. My dad is a trainer and for obvious reasons can’t get out and about at the moment so, we locked ourselves in a room for three weeks and committed his life’s work to film – which is now in the process of getting him up and running again!
As for myself, just before the crisis hit, I had started teaching twilight Pi-Top and Raspberry Pi sessions in schools and various other institutions. Again, this too has come to a (temporary) end, leaving me no alternative but to film my workshops and offer them up as pre recorded online training, the first of which is being filmed on Friday… by my tech phobic dad… it’s a good job I know how to teach him! So far I have received positive interest from Deaf Minds Education, Harlow Education Consortium and Parents and Autistic Children Together (PAACT)
 |
| My dad and sister in their Maker Masks |
Most exciting however was an email one Friday night from Pi-Top. Did I want to be involved with helping pi-top to create instructional videos for children to use when 3d printing respirator masks for the Maker Mask Movement. this involved printing some draft prints to see whether there was any parts that would be difficult for beginners or younger children.
Due to this being a huge success I then went on to print masks for many teachers, key workers and audiologists (my personal favourites) as well as one each for everyone in my family. As well as this, I am next week going to be continuing teaching raspberry pi and pi-top workshops digitally.
It really has been a busy time and I have been involved in all sorts of new and interesting things.
I can’t wait to see what happens next!
Stay safe
Isaac

Andrew Whitehouse is a specialist in neurological diversity and provides interventions for professionals, parents and young people with Autism, ADHD, Dyslexia and related conditions. Andrew has a number of roles including training, strategies and therapies for education professionals in schools and colleges, observing learners in the learning environment and providing practical solutions to help them achieve their potential. Andrew provides short courses for Bishop Grosseteste University and the University of Lincoln and holds a number of UK and overseas contracts. Andrew delivered a TEDx Talk “From Disability to Superpowers” and has an extensive conference profile. Andrew is also a Forensic SEND Consultant and acts as an expert witness in SEND related court cases.
During the Covid 19 crisis, Andrew is continuing to carry on his work by creating the online, social media project #GetInvolved collating and publishing bespoke blog posts by a range of high profile SEND professionals, running a wide range of free SEND workshops on Instagram, written and produced 27 online modular courses for London Borough of Sutton and delivered at a number of online conferences. Closer to home, Andrew is providing a lifeline telephone service for families of children with additional needs and co-hosts online Autism support group coffee mornings.
See Andrew’s TEDx here: https://www.ted.com/talks/andrew_whitehouse_from_disability_to_superpower
See Andrew at work here
https://www.youtube.com/watch?time_continue=4&v=XJ6FNQx-5ls&feature=emb_logo
My name is Sue Falkingham, by profession I’m an Audiologist, I work for Starkey Hearing Technologies as an Audiologist and a trainer. I’ve been an Audiologist for 30 years this year and I love it!
I’m also the Immediate Past President of the British Academy of Audiology, we are the biggest professional body for Audiology in the U.K. with most of our members working in NHS Audiology.
It became very clear whilst I was visiting an Audiology Department in Nottingham to do some training on 17th March that our lives were about to become very strange, for a significant amount of time. This was before the pubs, theatres and cinemas were asked to close and before we all went into lockdown. It was the last face to face piece of work I did.
So what happened?
That day the department received a message that they must cancel all their outpatient clinics for a month and must do it immediately, within minutes the messages were pouring into BAA as a group and individuals explaining similar emails and messages had been sent out to most NHS audiology departments in the country, with the cancellations to all routine clinics being for between 1 month and 3 months.
The feelings attached to a moment like that are immense and as an outsider watching a large group of people both in person and online react to that news was a very emotional thing. In one clinic it was 2,000 appointments in 4 weeks.
Shock, fear, anger uncertainty, concern a collective pulling on of the big girl and boy pants and doing what needed to be done became the order of the next few days.
By Friday schools, and pubs had been closed and on Monday 23rd the announcement that the whole country would go into lockdown happened but for those first few days I watched friends start to get to grips with what was a sudden announcement.
Audiologists are caring, concerned individuals who are problem solvers and scientists as well. As a profession we quickly understood the need to release capacity, to limit the amount of people in our NHS buildings and to protect our patients. Audiology in the main is not the frontline of the NHS but it is a vital service. We deal with often vulnerable people who have or develop problems with their hearing and balance systems.
So what is essential in Audiology and can we just stop all activity for up to 3 months?
Luckily nobody really wanted to stop all activity, what they wanted was to limit and if possible to stop all face to face contact, but nobody wanted people who rely on their hearing technology to communicate to stop getting repairs and batteries so they can remain connected and hearing through these challenging times. Departments all over the country started to share new ways of working, new ways of getting things to their patients, from standard postal services, to drop offs by car at patients homes when the audiologists were travelling in or out of hospitals, to local bicycle services for a more rural place. You can help maintain a 2m distance for this type of service easily.
The problem is at a safe 2m distance you can’t look in ears, you can’t take ear impressions and some of our testing gets difficult to do.
The first big piece of work I got involved with at BAA was around the testing of newborn babies who failed their hearing screening on the maternity units. Normally they have to come to an audiology service somewhere for more detailed testing and for potentially being diagnosed with life changing hearing loss. We normally want to test babies that fail the screen quickly, it reduces parental stress and allows any interventions we might want to discuss to be done at an early stage. The maternity screening programs are managed by Public Health England and are part of many tests done in Maternity, they are often very separate from Audiology services, Public Health England were a little busy and screening seemed to be a very small thing but we needed to get some clarity on how, when and by whom babies would be followed up. We initially put together a very small working group to write to PHE and express concern about baby screening and over the next 2 weeks that fabulous group worked with the screening managers at PHE to pull together guidance for services which was published on 30th March. The one thing the Corona Virus response has taught me is the speed things need to move at in health services has never been required before.
That small group of professionals is now conducting online meetings to answer questions that come up from individual locations and produce guidance for when we can switch back on our diagnostic services. It’s something we are hearing a lot about in this crisis but one of the questions for this group has been what personal protective equipment do you need to see a baby and be protected from Covid-19?
So now we have an immediate response but we then realised there is a lot of work to do as a Professional Body to try and support our members. We planned an online meeting of the Heads of Audiology Services, it gave over 100 people managing services a safe space to find out how other services were coping, what information was available and just to know that what they were doing was appropriate and similar to other places.
One thing has also become clear, audiologists have many transferable skills that can, during this period of crisis be put to use. So we started to see Audiologists being redeployed to other areas of the hospital. We’ve seen them retrained to test the fit of PPE, to safety test all the new ventilators and equipment coming in, to help staff from the frontline in wellbeing centres, to clean wards, to help in medical records, and to work in bereavement services. Audiology is part of the Healthcare Science Workforce and at times like these with rapid up skilling and supervision there are many skills we can put to use elsewhere.
Back in audiology departments a skeleton staff is still looking after their existing patients and seeing a few new emergency cases with ENT specialists. At BAA we initially released our own guidance on how services might do this safely and we have recently collaborated with other professional bodies to release a sector wide guidance.
It Also became clear that some patients were anxious thinking their usually audiology services were closed, they definitely are not. We started a social media campaign using messages from local NHS departments, sharing new ways of working, more direct support materials for patients and in some cases new contact and opening times. Look up our campaign using #StillHereForYou to see those great messages.
So what is happening to support this in my commercial “day job”? If a hearing aid needs fixing and the audiologist needs to send it to the manufacturer the manufacturers still need to be open. We have also adhered to best practices and most of our non production staff are working at home. In our factory a small number of staff go in to send out orders, manufacture new products and get them out to audiologists or direct to patients to help them continue to hear.
We have some really high tech production facilities and one of the things we are doing is “growing” children’s earpieces to fit their growing ears. Normally an audiologist might take a new set of ear impressions every month for their smallest patients, we would scan them and 3D print a new set of earmoulds. The audiologists can’t do that as they aren’t seeing the children face to face so we are adding a growth estimate to some of the scans we have on file for a child and making them bigger.if we don’t do that the children will have whistling hearing aids that will not help them hear.
Personally I am providing support and training to our customers on products online. Many of our high street customers have more time on their hands to learn as they are also only seeing people remotely, so it’s a great time to be productive and learn.
Many of my online conversations now revolve around what personal protective equipment audiologists will need to get back to face to face work. Generally we have never had to wear it before, generally good hygiene standards is all we have needed, does this have to change? If there is a global shortage of PPE what will audiologists be able to get and when is also a factor in returning to face to face contacts. The professional bodies need to put out more guidance and soon, so I’m also trying to start that piece of work with other interested bodies.
So what do I want to end this with? Audiologists are adaptable healthcare professionals. They are still able to help their patients mainly remotely and they will be back soon, rebooting their services and adapting to a new normal.
If you are worried about yours or a child’s hearing devices contact your normal NHS services and they will be there for you.
Stay safe
Stay home
And wash your hands
Sue
Connect with Sue on Twitter @swimto40
Connect with Starkey Hearing Technologies @Starkey_UK
For more than 20 years now I have been working with young people with neurological diversities such as Autism, ADHD, Dyslexia, Pathological Demand Avoidance Syndrome (PDA) and a range of related conditions. More recently, the focus has been on Social, Emotional and Mental Health (SEMH) and the links between SEMH and Neurological Diversity are plentiful. People who are perceived as being different, or indeed are different often feel like they don’t fit and struggle to achieve in a neurotypical world with neurotypical expectations.
So, my job… well I do a range of things. Conference presentations and keynote speeches, training workshops and insets and my favourite, observing young people in the learning environment – boots on the ground. This can be for a variety of reasons, challenging or disruptive behaviour, difficulties integrating socially, problems accessing the curriculum, not engaging with learning and a whole raft of other reasons. I have no particular system that I follow, other than, I follow leads. I look for what is going wrong and try to remove it from the equation or I look at what is going well and try to replicate it – “more of what works and less of what doesn’t. A sort of “Non-system system”.
See Andrew at work
So, based on observations I have carried out in the classroom, strategies I have found successful and interventions which have proved effective, I have put together the following list of eight ADHD friendly practices. I sincerely hope you find them useful.
Normalise ADHD
Young people with ADHD often feel that they are being judged for being different and not succeeding and yet there are so many positives. People with ADHD are good at lots of things. They can focus on the minutiae of tasks, they are creative problem solvers, they have boundless energy and yet often have low self-esteem. Talk about their ADHD, ask them about what they like about their ADHD, ask them what it is about their ADHD that causes them problems.
In through the eyes and out through the mouth
Give them opportunity to talk
People with ADHD find talking the quickest, most efficient way of communicating information and yet we can find them verbally intrusive, accuse them of interrupting. Try to make opportunities for your ADHD learner to talk. This brings us to…
Use your visuals
For the most part people with ADHD are visual processors and yet in my experience, most teaching is auditory verbal. Try to use your visuals more; visual timetables, now and next boards, lists of instructions, flash cards for spellings and any other visual interventions you can think of.
Remember attention spans #1
Depending on what you read, ADHD attention spans vary greatly. The theory I like to use is that a child’s attention span is there age plus a minute up until the age of 16. If that child has ADHD or a related condition, you can knock a third off that figure. So, an 8-year-old child with ADHD has potentially a 6-minute attention span, and yet may be expected to sit through a 20-minute assembly followed by a further 20 minutes on the carpet listening to teacher.
Remember attention spans #2
In contrast to what we have just discussed, if a child with ADHD is really interested in something, they can have an almost unlimited attention span. This has a knock-on effect on teaching and learning, if you can engage the child with ADHD’s interest, you will have great success, if you deliver non – contextual learning and teaching you will not gain their engagement.
A short video about attention spans
Gross/fine motor hyperactivity
Sitting still and not fiddling is not the natural state for people with ADHD and yet I see many professionals telling them to “leave that alone”, “put that down” and “stop rocking on your chair”. Try giving them something to fiddle with; hand putty, fidget cubes, fidget spinners etc and for gross motor hyperactivity try fidgety feet wobblers (an intervention I find useful – pictured). 
A short video about hyperactivity
Keep them busy
Staying busy works well for people with ADHD. Do you need a monitor for something? Do you need a personal assistant? Pencils need sharpening? Photocopying need doing? This is the ideal situation for a young person who finds sitting still a problem.
React/respond
Most teachers I work with agree that when working with young people with ADHD the hardest thing to manage is impulsive behaviour, in particular the tendency to react to situations without thinking through the repercussions. Spend time roleplaying situations that are either respond or react. Practicing this will prepare children to make the correct and appropriate choices in a range of situations.
Teaching a child with ADHD should not be difficult, just different. The problem with children with ADHD is not generally the ADHD but the expectation to behave neurotypically. With a few tweaks and some creative thinking, you will get significantly better results.
Let me know how you get on.

Andrew Whitehouse MSpEd CPSE (PGCert) BAHons QTS
SEN Consultant
TEDx Speaker
Bamford Lecturer
Adult with ADHD
07943838819
Aloha!
Welcome to #GetInvolved
Number 9 in a series of blog posts from my friends and colleagues in the education, health and care sector which I have been collecting and publishing over the last few weeks to help us all keep in touch.
Today’s post is by Gordon Forsyth from Parents and Autistic Children Together: PAACT Support. I have had the pleasure of supplying training workshops to parents and professionals through PAACT since 2016 and during that time I have learned that Gordon is totally committed to supporting young people with additional needs, as well as their families and the professionals that work with them.
Today, Gordon would like to offer you a lifeline…
Lets Get Talking
While we are entering the end of the third week of lock down has the novelty of being at home instead of going to work or school gone, if it was there in the first place.
Maybe our children are just not able to keep up day to day learning as we are hearing from lots of people from TV to FB showing how clever they are at being wonderfully creative and how well their children are coping.
My daughter’s response to that is, “good luck if you think I am doing that”.
This then sets us as parents a challenge as how do we get our children to do their work, we are exhausted and coming up with creative fun ways to ensure they get some learning done during the day feels like an expedition up Mount Everest and we have fallen at the phone call stage of planning.
This then makes us feel down why can I not get my child to engage, we tell them they must do what has been set for them, you can not stay in bed and no you are not going on Xbox again. We then get our daily response of sorry mum /dad, I just am not able to do it today or something similar to this but probably much more colourful.
We now feel the pressure, what should we do? How do we deal with this?
Then we have the boredom of nothing to do, why can’t we go out, or why can’t I play on my Xbox or watch the telly anything but what you would like them to do.
We may start to have a meltdown ourselves by raising our voices banging things down, saying out loud why can’t you just do as I ask for once, is it really that difficult, No, just me, thought so.
Our child/ children then have to cope with the change of lots of people in the house with much more noise and people making demands that have not happened in this way before.
Siblings getting on with each other has never been easy but manageable to a degree as they are mainly at school so you have a bit of respite, not now as at least one of your children or your only child wants to be in total control and in their eyes is running the show. So as we know we just let them do what they want, yes!!
Anxiety has now taken over the whole house as we are walking on eggshells we are now chief negotiators for family peace and no sign of bed time for us or our children, panic is now setting in and we start to doubt our ability to cope as the day is getting too hard and I am a terrible parent and just maybe the professionals were right I am a bad parent.
At this point we have lost perspective of what is really happening, we have given in to our years and years of programming of how things should be done and they will be done when I say etc etc.
If any of this sounds familiar and it should as you are not alone going through the same battle and feeling you are not coping. I will say this, you are all doing so well as you are all doing your best to get through the day the best way you know.
Due to the coronavirus PAACT had to stop their monthly support meetings and this for me was a huge resource and good night or morning out to meet other parents going through similar things to me and they had a different idea on how to deal with a situation or confirm we are going through the same issue and no matter what we do nothing seems to work.
This discussion is priceless as it boosts your own confidence makes you feel better about yourself makes you feel empowered and helps to understand what your own child might be struggling with and gives you a better perspective or understanding and therefore reduces your anxiety which in turn will reduce their anxiety.
Stopping the support meetings gave me the biggest worry as I know we need to provide support for families but with my non existent technical knowledge I was anxious on how to get the support meetings to work again.
I got in touch with Andrew Whitehouse and asked him for help and he very kindly told me he was putting his amazing workshops ( my words not his) onto Instagram Live so information could get out and hopefully help getting to understand there is no answer but small steps small victories for us to build upon.
By talking with Andrew and other members of PAACT I feel we are now in a position to go live with support meetings on a weekly basis with the first one taking place on Tuesday 14th at 2:00pm. After this one we can look at alternating the meetings from morning, afternoon and evening depending on what you feel would work best.
Being able to talk and hear what other families are doing will help us all. I have been going to support meetings for the last 14 years and I always come away with really good information and advice that I have not heard before or hearing something from a different perspective that makes such a difference to our family.
For more information about this please email me at paactsupport@hotmail.co.uk
Join me today, Tuesday 14th at 2:00pm (if you can’t join today, please be assured – there will be more).
Let’s get talking
Gordon Forsyth,
PAACT Support

-
Have you lost your day services or respite care?
-
Are you in survival mode, just trying to get through each day at a time?
-
Are you finding that time is dragging and you’re struggling to find things to do?
How to survive lockdown with a child or young adult with additional needs – Neale Hayward-Shott
Read how Fliss has found her routine and settled into daily home learning
The Weekly Visual Timetable
On the 25th March, my daughter, Fliss, came home from her day centre for the last time for a while.
At first, she was quite unsettled as she enjoys her routine and is very fond of her support workers. Fliss is very attached to her weekly visual timetable and refers to it frequently to ground her. She likes to know what she’s doing each day of the week. Being in lockdown, at home all the time, had taken away the structure that she found reassuring.
Fliss has learning disabilities and can’t process information easily unless it’s clear and, in her case that means, visual.
So, we needed to create a new structure to replace the one that she’d lost. We created a list of topics (see the list at the bottom of the article for reference), selected a photo for each topic and printed all the pictures. Fliss then selected the topics that she wanted to start with and put them into the pockets that she uses with her weekly visual timetable.

To add to the topics, and create more variety, she then chose pictures of people that she could email or phone on certain days. We don’t do the topics at the weekend as we try to keep the weekday / weekend difference.
Other people that I have suggested this idea to have chosen different countries or animals for the topics. Use whatever your child is interested in. Deciding what to do each day without a plan is like having a blank piece of paper staring at you when someone tells you to write an article. Once you have the topic things are much easier. Once you have a topic you can search for craft ideas, pictures, puzzles, videos and all sort of activities. If you would like a copy of my pictures, then email me at the address below.
The Daily Personal Planning Board
Having a weekly visual timetable is a good start and really helps with the big picture. But keeping someone with a learning disability engaged all day can be difficult. Now I have to say, at this point, that the daily home learning is down to my wonderful wife, Heather. Each morning Heather helps Fliss to set up her Personal Planning Board with the various activities for the day.
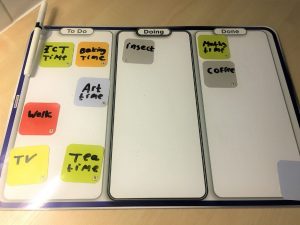
Fliss writes each of the different activities for the day on one of the Gecko dry-wipe notes that come with her board. Some activities are the same each day, some are new and every day includes the focus topic. At the start of the day, and at the start of each new activity, Fliss will chose one of the activities and move the note from the To Do column to the Doing column. At some points in the day she can choose whatever she would like to do next and at other times her choice is guided. After the activity is finished Fliss moves the note over to the Done column.
Working through the Personal Planning Board in this way gives Fliss a visual idea of what she has achieved so far and what is left to do. It also helps her to recount the day and tell other family and friends about what she’s done. Without the board that’s something she really struggles to do.
It’s very hard work supporting someone with an additional need all day every day. For Heather and Fliss’ the OurBoards Weekly Visual Timetable and OurBoards Personal Planning Board bring structure, engagement, understanding and a lack of anxiety to home learning.

Neale is the founder of OurBoards Community Interest Company
Contact details:
Neale Hayward-Shott
neale@OurBoards.co.uk
http://OurBoards.co.uk
Topics that Fliss is working through
Flowers, Trees, Houses, Dogs, Horses, Fields, Cars, People, Food, Churches, Fences, Post boxes, Drinks, Farms, Walls, Birds, Insects, Boats, Trains, Planes, Rivers, Ponds, Beaches, Woods & Forests, Space, Water, Desert, Arctic, Butterflies